Your Pregnancy Help Organization and COVID-19
If you are a Heartbeat Affiliate, please click log in at the top of the page to view more materials! Additional materials will appear below for those current affiliates who are already logged in. Click here for more information about affiliating with Heartbeat International.
You can also get a recording of our webinar series Coronavirus and Your Pregnancy Help Organization for free by clicking here. Resources related to those webinars are also available on the Complimentary Materials page here.
The information in these articles is accurate as of the publication date of each one. We are working to keep our articles up-to-date as changes surrounding COVID-19 occur, and we encourage everyone to check the CDC, WHO and their local authorities as the situation is ever-evolving.
Displaying items by tag: fetal development
What You Need to Know About the Dangers of Prenatal Tests
By Susan Dammann, RN, LAS, Medical Specialist
Reporting in Prenatal Tests: What Patients Should Know published in Medscape News and WebMD, Kathleen Doheny described a recent investigation revealing there are significant inaccuracies in non-invasive prenatal screening and that some women and doctors are misinterpreting the positive results from the new generation of prenatal tests including MaterniT21Plus, Verifi, Panorama and Harmony. In some instances, women are terminating their pregnancies because of it. This decision appears to be based on the screen alone without obtaining tests to confirm a negative diagnosis.
Beth Daley from the New England Center for Investigative Reporting in an excellent article Overused and Misunderstood stated "a three-month examination by the New England Center for Investigative Reporting has found that companies are overselling the accuracy of their tests and doing little to educate expecting parents or their doctors about the significant risks of false alarms."
"All claim to offer expectant parents the chance to know with almost 100% accuracy, and as early as 10 weeks into a pregnancy, the likelihood that the developing baby has any genetic abnormalities such as Down syndrome, Edwards syndrome (trisomy 18), Patau syndrome (trisomy 13), or a few other chromosomal anomalies" writes Nora Sullivan with the Charlotte Lozier Institute in her article Non-invasive Prenatal Screening Expands Disability Discrimination Abortion.
Daley goes on to say: "A screen is a test given to a general healthy population and usually has high sensitivity so that any possible problems are flagged. Because of the high sensitivity, false positives are more common. Also, screens are not necessarily approved by the FDA. Because of a loophole from the 1970's, these types of screening tests are not subject to the same regulation as other medical devices or procedures. A screen is always supposed to be confirmed with a diagnostic test. A diagnostic test is designed with high specificity for a particular condition flagged by the screen. It is often more invasive and is meant as a tool to make a definitive diagnosis."
The problem appears to be not understanding a "statistical blip" in how the test results are reported or what is called "positive predictive value". What is critical for both health care providers and patients to understand is that the test is a "risk-based test" not a diagnostic test and a positive test result is only indicative that they have a higher risk of having that particular issue. The article reported that in the general population of women, a well-regarded study published in the New England Journal of Medicine showed that the test was correct for only about 40% of women who tested positive for Edwards syndrome (trisomy 18).
Daley said, "If companies are presenting these screens to be as good or better than a diagnostic test, doctors believe them and parents are aborting as a result, then the companies are seriously negligent."
Therefore if a patient comes into a pregnancy center considering abortion if/because test results come back positive, it is important to educate the patient that this test is only a screening for risk. A positive result is only an indication that their risk may be higher, but the test result could be wrong and a confirmatory test like a CVS (chorionic villus sampling) or an amniocentesis is needed to be sure. A patient should always get a confirmation with an FDA approved diagnostic test.
Aborting a child due to a genetic abnormality is disability discrimination. Prenatal tests should never be used for such purposes. When a disability is discovered rather than termination, options for the provision of treatment or hospice care should be offered.
Armed with the information above, we can help women who may be determined to abort due to a negative diagnosis to get further testing for verification. This will facilitate additional time to help them with alternative options should the diagnosis be positive.
Experts to Help! Pro-Life Maternal-Fetal Medicine Docs
Two important resources for your center and medical director
 |
by Susan Dammann RN, Medical Specialist
Dedicated to the care and preservation of both mother and fetus in every pregnancy, Pro-Life Maternal Fetal Medicine (MFM) is an association of pro-life doctors of like mind to AAPLOG (American Association of Pro-Life Obstetricians and Gynecologists).
This unique organization represents a contingent of life-minded Maternal Fetal Medicine (MFM) practitioners. (MFM is a subspecialty of Obstetrics and Gynecology dealing with all matters that can affect the health of a mother or fetus from before conception to the postpartum period.)
Members of Pro-Life MFM are also affiliated with the Society for Maternal-Fetal Medicine, a special interest group of the American College of Obstetrics and Gynecology who have received additional training and performed research in the care and management of pregnant women and fetuses.
The Role of Pro-Life MFM Practitioners
MFM professionals are specialists in high-risk pregnancy situations, and hold a uniquely expert place in relation to rank-and-file OB/GYN physicians or oncologists. MFM specialists are involved in guiding the management of medical and surgical complications a mother may encounter during pregnancy.
MFM specialists also provide diagnosis and management of medical and surgical conditions for the fetus. Care may include in utero treatment, modification of delivery timing or mode, and facilitation and coordination of care for the infant after delivery.
When a client presents in your center with a negative maternal or fetal diagnosis, there are alternatives to help ensure the survival of both mother and baby. For example, many women with a breast cancer diagnosis have carried their pregnancies to term and done better than women who abort.
Are you looking for a pro-life Maternal-Fetal Medicine specialist in your area? Visit Pro-Life MFM’s physician directory.
Hear from a Pro-Life MFM Expert
Dr. Murphy Goodwin, a well-known pro-life maternal fetal medicine specialist, wrote an excellent article called Medicalizing Abortion Decisions. Dr. Goodwin, whose obstetric practice in the Los Angeles area has been the largest in the United States for most of the last 15 years, serves many of the high-risk deliveries in the area.
While describing five cases of successful delivery where a mother had abortion recommended to her, Dr. Goodwin states that because of the dangerous combination of an ambivalent attitude toward the developing human in the medical community and fear of liability issues (owing to the unbalanced legal burden of informed consent and “wrongful birth”), physicians are often not providing readily available information that could affect their patients’ judgment regarding abortion when that mother has a major medical problem in pregnancy or any medical problem.
To suggest or recommend that abortion is the safest route carries no such responsibility, as there is no set legal precedent for a physician’s liability in a case where abortion was recommended on supposed medical grounds—even if that recommendation was subsequently found to be baseless or misrepresented.
Tragically, as Dr. Goodwin points out, “There is no counterweight to ‘wrongful birth.’ There is no ‘wrongful abortion.’
These are two helpful resources you’ll want to keep handy and make available to your medical director!
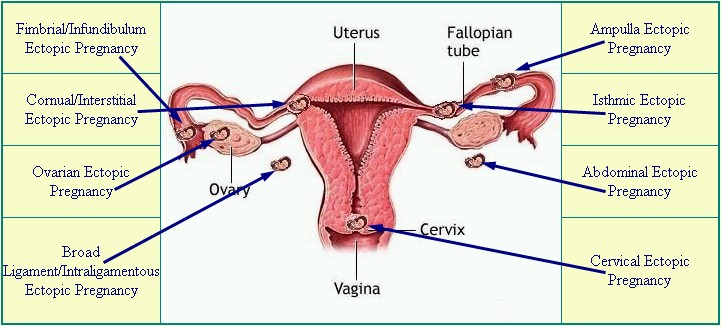
Get up to Speed on Ectopic Pregnancies
|
Diagram from EctopicPregnancyFoundation.org |
By Susan Dammann, RN, Medical Specialist
Ectopic pregnancies occur in a range of 1 in 40 to 1 in 100 pregnancies. An ectopic pregnancy is any pregnancy that implants somewhere outside of the uterus, most often occurring in one of the fallopian tubes, which is also known as a tubal pregnancy. Other locations for an ectopic pregnancy include the ovary, the cervix, and the abdominal cavity.
Ectopic pregnancies are life-threatening for the mother, and the baby (embryo) cannot survive. Ectopic pregnancies may occur with or without the use of birth control.
Though rare when considered with the overall number of U.S. pregnancies, ectopic pregnancies still occur at a rate of 100,000 per year, according to the Center for Disease Control. The CDC also reports the life-threatening nature of an ectopic pregnancy for a mother: "Ectopic pregnancies are the leading cause of pregnancy related deaths in the first trimester and account for 9% of all pregnancy related deaths in the country."
Causes
An ectopic pregnancy can result from any condition blocking or slowing the movement of the embryo through the fallopian tube, where it then becomes lodged. The cause, sometimes unknown in an individual case, may include any of the following:
- Tubal damage resulting from sexually transmitted infections
- Inflamed, damaged or misshapen fallopian tube
- Hormonal imbalances
- Abnormal fetal development
- Complications/scarring after a ruptured appendix
- Endometriosis
- A previous ectopic pregnancy
- Scarring from past infections or surgery of the female organs
- Illicit drug use (“An alarming increase in ectopic pregnancy-related deaths among Florida women is likely caused by illicit drug use and delays in seeking medical care…”)
Risk Factors
- Having had many sexual partners
- Surgery to reverse a tubal ligation
- IUD in place
- In vitro fertilization
- Over 35 years of age
- Some infertility treatments
- Tubal ligation (more likely 2 or more years after the procedure)
Symptoms
Initially, an ectopic pregnancy may not cause any symptoms outside of those of a normal pregnancy. A pregnancy test will read positive, but will likely be accompanied by the following symptoms:
- Abnormal vaginal bleeding—heavy vaginal bleeding is not likely unless the ectopic pregnancy is in the cervix
- Pain in the lower belly or pelvic area
- No period
- Low back pain
- Cramping on one side of the pelvis
If the areas around the ectopic pregnancy rupture and bleed, symptoms may worsen and include:
- Low blood pressure
- Pain in the shoulder area, due to blood leaking from the fallopian tube
- Urge to have a bowel movement, due to blood leaking from the fallopian tube and pooling
- Severe, sharp, and sudden pain in the lower abdomen
- Fainting or feeling faint
Complications
- Unless treated, a ruptured fallopian tube may be life-threatening
- Shock
- Infertility
Diagnosis
If an ectopic pregnancy is suspected, the physician may do a pelvic exam to check for pain. Tenderness or a mass in the fallopian tube or ovary may be an indicator. Blood tests and vaginal ultrasound exam help confirm the diagnosis, as does checking hCG blood levels over 1 to 2 days.
[Related—Transvaginal Sonogram: Is it Necessary in Your Center?]
Ectopic pregnancy may occur after tubal ligation, even more so if the woman was sterilized before 30 years of age. One study found these women were twice as likely to have a subsequent ectopic pregnancy as those women who undergo tubual ligation after the age of 30. It should never be assumed that a woman’s history of tubal ligation automatically rules out the possibility of an ectopic pregnancy.
Treatment
In order to prevent the loss of a mother’s life in addition to the loss of her embryo, intervention is required. The pregnancy cannot continue to full-term. If the ectopic pregnancy is diagnosed before symptoms occur, treatment may consist of an injection of methotrexate to stop cell growth. Ectopic pregnancies can be removed through laparoscopic surgery. If the fallopian tube is damaged, it may need to be removed as well.
Emergency medical attention is required if the fallopian tube has ruptured and heavy bleeding is occurring. Emergency surgery (laparotomy) may be required to stop the blood loss, as well as the termination of the pregnancy and possibly removal of the fallopian tube. Because the rupture can lead to shock, the following may be necessary:
- Blood transfusion
- Intravenous fluids
- Oxygen
- Trendelenberg position
- Added warmth
Prognosis
While some women do not conceive subsequent to an ectopic pregnancy, approximately one-third do experience a later pregnancy. Of this one-third who do become pregnant following an ectopic pregnancy, approximately one-third will have a repeat ectopic pregnancy.
Prevention
The best means of avoiding a tubal pregnancy is to avoid anything that would cause infection, or scarring of the fallopian tubes. Early diagnosis and treatment of all STD/STIs is critical. There are, however, no preventative measures to avoid ectopic pregnancy occurring outside the fallopian tubes.
Patient Instruction Sheet
This information is critical for pregnancy center staff to know. With every client who comes in our center with a positive pregnancy test we must be aware that she could potentially have an ectopic pregnancy. Therefore, it is recommended every center have a policy and procedure for advising clients of the signs and symptoms of an ectopic pregnancy.
This could be as simple as giving your client a sheet of instructions and information listing the signs and symptoms of an ectopic pregnancy, along with instruction to contact a health professional immediately if she experiences any of these symptoms.
Sources:
1. http://www.mayoclinic.com/health/ectopic-pregnancy/DS00622
2. http://www.nlm.nih.gov/medlineplus/ency/article/000895.htm
3. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001897/
Tubal pregnancy; Cervical pregnancy; Tubal ligation-ectopic pregnancy
4. CDC Fact Sheet: Ectopic Pregnancy Risk after Tubal Sterilization
[CDC Reproductive Health Information Source, 7/04 http://pregnancy.about.com/cs/ectopicpregnancy/l/bltubalfacts.htm]
5. http://health.usnews.com/health-news/news/articles/2012/02/16/illicit-drug-use-may-be-driving-rise-in-ectopic-pregnancies-in-florida
Birth Defects: Get Help, Get Connected
Four Helpful Sites
While this is not an exhaustive list, listed below are some references you may want to investigate as possible resources for your center to offer clients with a poor prenatal diagnosis.
- It’s a Mom’s World – Special Needs provides support and information for a mother or couple whose child is diagnosed with special needs.

Samuel Armas -- 21 weeks in utero (FoxNews.com)

Samuel Armas -- 9 years old
(FoxNews.com) - Prenatal Partners for Life is “a group of concerned parents (most of whom have or had a special needs child), medical professionals, legal professionals and clergy whose aim is to support, inform and encourage expectant or new parents. We offer support by connecting parents facing an adverse diagnosis with other parents who have had the same diagnosis. We have many resources such as adoption agencies with clients waiting to adopt and love a special needs child should a parent feel they could not care for them.”
- IsaiahsPromise.net is “a group of parents who knew early in our pregnancies that our babies had severe or fatal birth defects. Each of us, for various reasons, continued the pregnancy. It's a difficult and very personal decision. We know the devastation, confusion, heartbreak and loneliness. We can't change your circumstances or make decisions for you. But we can offer support, friendship and experience.”
- BeNotAfriad.net is “an online outreach to parents who have received a poor or difficult prenatal diagnosis. The family stories, articles, and links within this site are presented as a resource for those who may have been asked to choose between terminating a pregnancy or continuing on despite the diagnosis. The benotafraid.net families faced the same decision and chose not to terminate. By sharing our experiences, we hope to offer encouragement to those who may be afraid to continue on.”
Free Symposium
The First Annual Conference on Medical Advances in Prenatal Diagnoses was hosted by the Council on Poor Prenatal Diagnoses & Therapeutic Intervention in January of 2012.
The conference brought together professionals from many different specialty areas, including genetic researchers, ob-gyn physicians, developmental pediatricians, hospital nursing staff, medical genetic counselors, and medical students. Other participants and guests included peer ministry providers, social service support professionals, advocates for persons with disabilities and public policy specialists.
Julie Armas and her son, Samuel, both spoke at the conference, testifying to the wonderful life Samuel has lived, even with a prenatal diagnosis of spina bifida. The unforgettable 1999 picture of Samuel’s tiny finger reaching out of the womb and grasping his surgeon’s finger was printed in several newspapers worldwide, including USA Today. Samuel turned 13 in December of 2012.
You can view this full-day conference free of charge here.
Birth Defects Fact Sheets
 While there are thousands of different birth defects, the most common are heart defects, cleft lip and cleft palate, Down syndrome and spina bifida. Approximately 150,000 children are born every year in the United States affected by one or more birth defects, according to the American Pregnancy Association.
While there are thousands of different birth defects, the most common are heart defects, cleft lip and cleft palate, Down syndrome and spina bifida. Approximately 150,000 children are born every year in the United States affected by one or more birth defects, according to the American Pregnancy Association.
The CDC reports that one in every 33 babies (about 3 percent) is born with a birth defect, and that birth defects are one of the leading causes of infant deaths, accounting for more than 20 percent of all infant deaths. Causes vary, including the use of alcohol, street drugs, and prescription drugs, being exposed to various infections such as cytomegalovirus or sexually transmitted infections. Genetic conditions can also be passed from parent to child.
Information about Specific Birth Defects
The CDC has great information on many birth defects which you may find useful in your center at the following links:
- Anencephaly
- Cleft Lip / Cleft Palate
- Congenital Heart Defects
- Down Syndrome
- Encephalocele
- Gastroschisis
- Hypospadias
- Omphalocele
- Spina Bifida
- Upper and Lower Limb Reduction Defects
 Cytomegalovirus (CMV) Disease: The Congenital Disease Mothers Don't Know About
Cytomegalovirus (CMV) Disease: The Congenital Disease Mothers Don't Know About
The following information is also found at the CDC site:
CMV is the most common congenital (present at birth) viral infection in the U.S. Each year, about 5,500 (1 in 750) children in this country are born with or develop disabilities that result from congenital CMV infection. More children have disabilities due to this disease than other well-known congenital infections and syndromes, including Down syndrome, fetal alcohol syndrome, spina bifida, and pediatric HIV/AIDS.
CMV is spread from person to person by close contact with body fluids, such as blood, urine, saliva, semen, vaginal fluids, and breast milk. Once CMV is in a person's body, it stays there for life. Most people who become infected with CMV have mild, flu-like symptoms or no symptoms at all; the exceptions are infants with congenital infection or people who have weakened immune systems.
For pregnant women, sexual contact is a common source of CMV infection. Limiting sexual partners and practicing safe sex may reduce the risk of catching CMV.
Another common source of infection for pregnant women is contact with the urine or saliva of young children who are infected with CMV and are shedding the virus.
Tips to Get a Fetal Heart Beat
By Kimela Hardy, MA, RT(R), RDMS
Available literature states the fetal heart beat begins its lifelong work at approximately six weeks, and depending on the sonographer’s skills, ultrasound system, and maternal body habitus, the heart beating may be visualized at this time. There are several factors that can be used to not only see this little miracle at work, but also improve general images.
Back to the Basics of Ultrasound
|
Thermal Index is the heating of tissue as ultrasound is absorbed by tissue, measured by ratio of power used to produce a temperature increase of 1°C. This is measured in soft tissue (TIS), bone (TIB), and in the cranium (TIC). The Mechanical Index is an ultrasound measurement used as estimation of the risk of non thermal effects and the degree of bio-effects a given set of ultrasound parameters will induce; Higher MI means a larger bio-effect. These can include cavitation, the formation of transient or stable bubbles, which can damage tissues. The current Federal Drug Administration has set the maximum MI at 1.9 MI = PNP Peak Negative Pressure of the ultrasound wave |
Before a specific organ, for example the fetal heart, image can be improved on, first obtain the best image possible. To begin any ultrasound study, but especially in Obstetrical scanning, the correct manufacturer’s Preset must be selected. Presets are essentially a “recipe” set for the ultrasound system. These parameters may include depth, gain, frequency, and focus among other factors. Using the OB Preset sets the Thermal Index (TI) and Mechanical Index (MI) which are generally lower for obstetric ultrasound examinations. In general, the TI and MI are not deliberately manipulated during routine ultrasound examinations.
Which Knobs Can Improve Your Picture?
Once the Preset is selected, consider the overall gain in the image on the monitor. Is it all black, all white, or a combination with many grays? Adjust the overall gain, often a large dial easily accessible, so it is easiest to identify the landmarks and in general is appealing to one’s eye and interpretation. This may differ somewhat with each sonographer, but not to an extreme.
The importance of correctly interpreting the landmarks cannot be over stressed, know the anatomy well.
Be sure the size of your image, or depth, allow demonstration of the area of interest. On some machines, this is either a dial knob or toggle switch labeled Depth, Size, or a combination of these. There is a scale on either side of the image that registers this depth in either centimeters or millimeters, and changes as the dial/toggle is adjusted.
Most transducers/probes are multi-herz, which means they offer more than one frequency, usually 2, 4, and 6 MHz. Once the landmarks have been identified and the overall gain is satisfactory, try each frequency with a simple adjustment and determine which provides the best penetration and resolution.
Remember:
- The lower the frequency, the higher the penetration but lower the resolution.
- The higher the frequency, the less the penetration but the better the resolution.
This means images of a patient with Large Maternal Body Habitus (LMBH) most often improves with the lowest frequency, and our smaller, more athletic patients can use the higher frequency for better resolution images. The frequency is often displayed at the top of the image where the TI and MI are located.
The optimal area of the ultrasound beam is the focus, demonstrated by a triangle or karat along the depth scale. Place this at the area of interest at the correct depth. On some systems, the focus makes a significant difference in clarity, but in other systems, there does not appear to be much change.
After the above have been set to optimize the image, the slide pods or TGC/STC can be used to fine tune the image even more. These are a step alteration in the gain, with the slides on the top affecting the top of the image and vice versa. Most often the “slope” is a gradual downward slope to the right.
Manufacturers frequently have specific image enhancing features under proprietary names which reduce haze, clutter, and artifacts allowing for improved clarity of images. These harmonic features may allow for increased penetration without details lost. Simply turning this feature on and determining its benefit (or not) is required.
Looking at the Heart
Once the optimal image has been achieved by using the features discussed above, there are additional tips to see that small fetal heart.
Some systems have a Field of View (FOV) which has the effect of “coning down” and creating a smaller field visible and increases image clarification. This is the consequence of taking only a portion of the available area to scan instead of the entire area seen prior to using this option. Often, a pie-shaped icon is on the image top to illustrate and highlight the FOV area.
Using the Zoom option will increase the image size, which also can make it easier to visualize the fetal heart. In addition, most of the Zoom also has a feature which allows the size of the area, or box, to be increased/decreased. Another key to using a zoom option is to be certain the item of interest is directly in the center of the box.
When viewing the small fetal heart, another gain adjustment making the image brighter aids in recognizing the wave form during Motion-mode (M-mode). This gain is sometimes located by turning the M-mode dial. The brighter the image, the more likely the wave form is visualized. Also, the wave form will be in direct relationship to the location of the heart in the 2 Dimensional (2 D) image. For example, if the heart is in the center, the q, r, s, etc. waves will be in the center of the strip. If the heart is at the bottom of the image, the wave form will be at the bottom of the strip.
Oftentimes, maternal respirations interfere with achieving a well demonstrated strip. To overcome this, ask the patient/client to suspend breathing or hold her breath. Be aware, if she takes in a deep breath, the fetal heart may move out of the image, and you will need to make the necessary adjustments.
All of these discussed options to improve ultrasound images pertain to both Transabdominal and Transvaginal imaging. However, it is reasonable to anticipate that Transvaginal images will be larger and therefore improve the ability to obtain a fetal heart rate.
Using these tips should increase the skill set and confidence for the nurse sonographer and show this little miracle to his or her maximum potential. The tips prior to the “M-mode” can be used for general imaging as well.